Assessing Family Involvement in Early Psychosis Recovery: A Descriptive Analysis of Demographic Patterns in Boston Medical Center’s First-Episode Psychosis Program
Julie Ngo BA (1,2), Amelia Blanton BS (2), Berneece Tam BS (1), Brittany Gouse MD (2), Hannah Brown MD (2)
1. Boston University Chobanian & Avedisian School of Medicine
2. WRAP Research Program, Boston Medical Center, Boston, MA
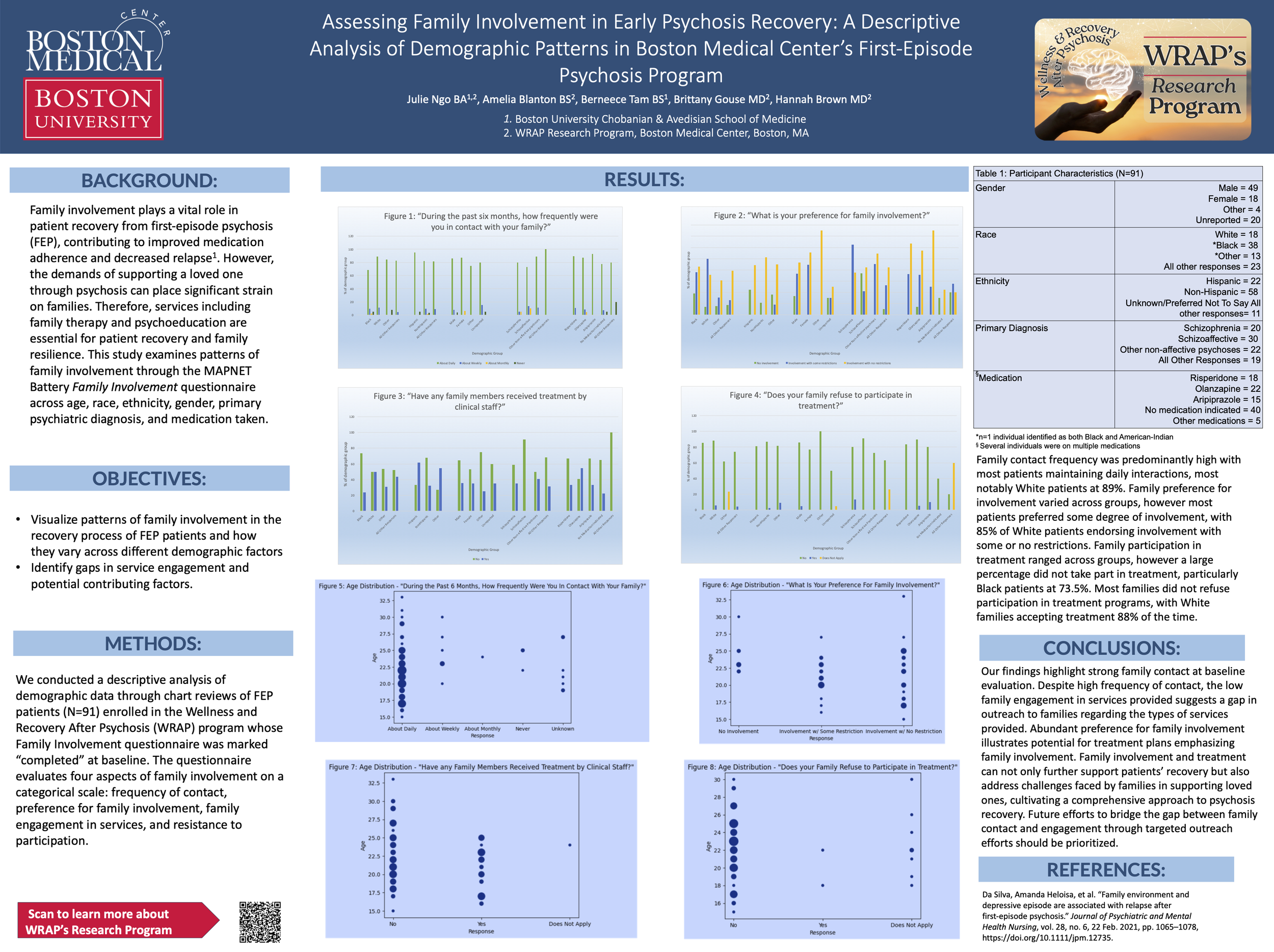
Background: Family involvement plays a vital role in patient recovery from first-episode psychosis (FEP), contributing to improved medication adherence and decreased relapse1. However, the demands of supporting a loved one through psychosis can place significant strain on families. Therefore, services including family therapy and psychoeducation are essential for patient recovery and family resilience. This study examines patterns of family involvement through the Family Involvement questionnaire across race, ethnicity, age, gender, and primary psychiatric diagnosis.
Methods: We conducted a descriptive analysis of demographic data through chart reviews of FEP patients (N=230) enrolled in the Wellness and Recovery After Psychosis (WRAP) program whose Family Involvement questionnaire was completed at baseline. The questionnaire evaluates four aspects of family involvement on a categorical scale: frequency of contact, preference for family involvement, family engagement in services, and resistance to participation.
Results: Family contact frequency was predominantly high with most patients maintaining daily interactions, most notably White patients at 89%. Family preference for involvement varied across groups, however most patients preferred some degree of involvement, with 85% of White patients endorsing involvement with some or no restrictions. Family participation in treatment ranged across groups, however a large percentage did not take part in treatment, particularly Black patients at 73.5%. Most families did not refuse participation in treatment programs, with White families accepting treatment 88% of the time.
Conclusion: Our findings highlight strong family contact at baseline evaluation. Despite high frequency of contact, the low family engagement in services provided suggests a gap in outreach to families regarding the types of services provided. Abundant preference for family involvement illustrates potential for treatment plans emphasizing family involvement. Family involvement and treatment can not only further support patients’ recovery but also address challenges faced by families in supporting loved ones, cultivating a comprehensive approach to psychosis recovery.