Validation of a brief psychosis screener in a population seeking help through the Massachusetts General Hospital Psychosis and Clinical Research Program
Cheryl Y. S. Foo, PhD* (1,2), Jacqueline Clauss, MD, PhD* (1), Lauren Utter, PsyD (1), Drew Coman, PhD (1), Michaela Newton, MA (1,3), Abigail Donovan, MD (1), Corinne Cather, PhD (1,2), Daphne Holt, MD, PhD (1)
1. Psychosis and Clinical Research Program, Department of Psychiatry, Massachusetts General Hospital 2. Center of Excellence for Psychosocial and Systemic Research, Department of Psychiatry, Massachusetts General Hospital
3. Clinical Psychology Department, William James College
*Authors contributed equally.
Abstract
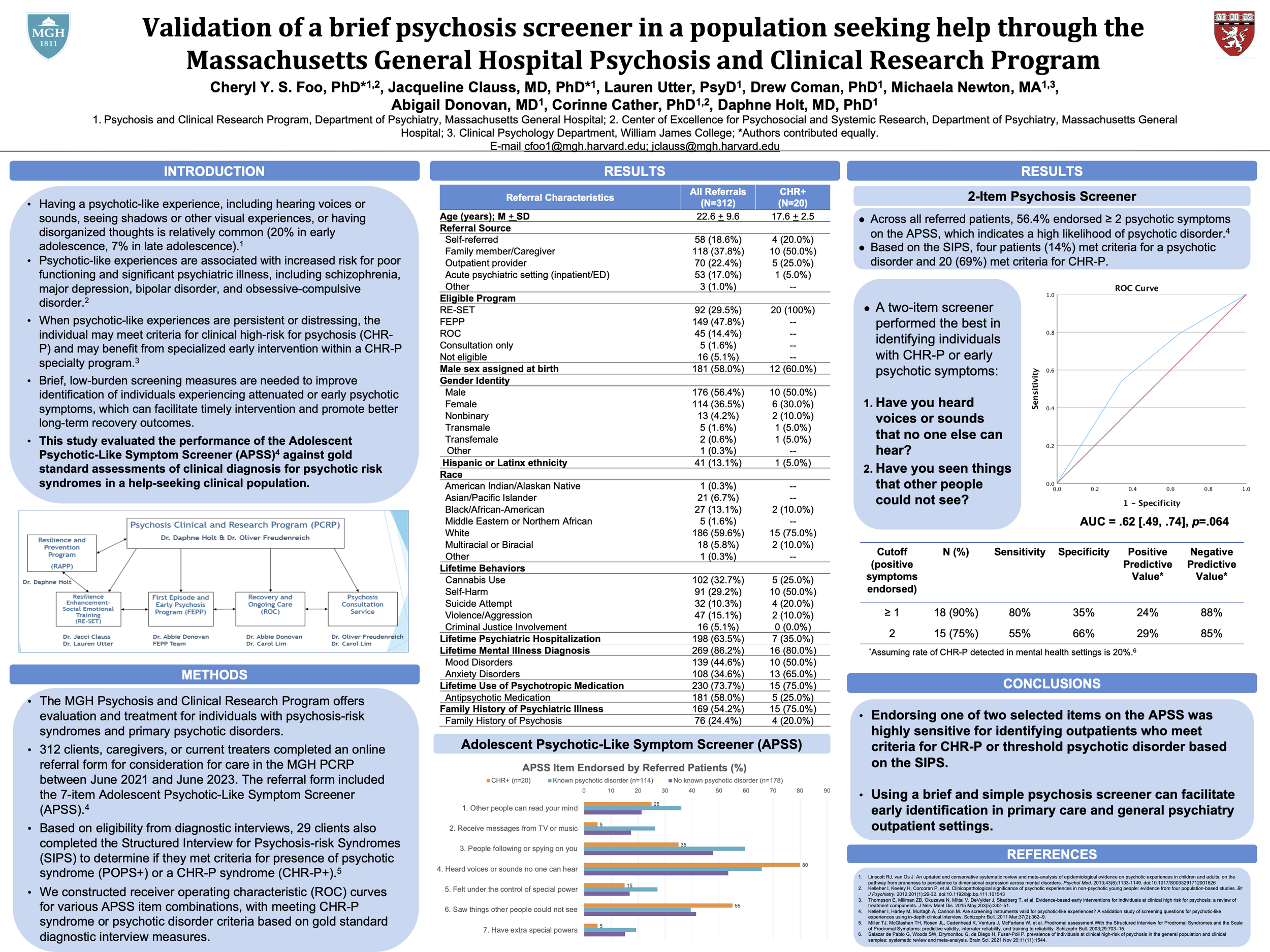
Background: Attenuated psychotic symptoms are relatively common and are associated with increased risk for a range of psychological disorders including, but not limited to, schizophrenia. In Massachusetts, only approximately 1-2% of individuals at clinical high risk for psychosis (CHR-P) receive treatment in specialized programs. Brief, low-burden screening measures are needed to identify individuals experiencing attenuated or early psychotic symptoms, which can facilitate timely referral to specialty psychosis treatment programs to promote better long-term symptom and recovery outcomes.
Methods: The MGH Psychosis and Clinical Research Program offers evaluation and treatment for individuals with psychosis-risk syndromes and primary psychotic disorders. A total of 312 individuals completed an online screening form that included the 7-item Adolescent Psychotic-Like Symptom Screener (APSS) between June 2021 and June 2023. We evaluated the performance of the APSS items against gold standard assessments of either CHR-P or primary psychotic disorder based on clinical diagnostic interviews and/or the Structured Interview for Psychosis-risk Syndromes (SIPS).
Results: 29 (9.3%) referrals were clinically indicated for a SIPS assessment for CHR-P. Based on SIPS criteria, 4 (1.3%) met criteria for psychotic disorder and 20 (6.4%) met criteria for CHR-P. Endorsement of at least one positive symptom on a two-item screener (auditory or visual hallucinations) derived from the APSS identified individuals with CHR-P or primary psychotic disorder with 79% sensitivity and 35% specificity, AUC = .61 [.50, .73], p = .066.
Conclusion: A two-item version of the APSS was highly sensitive for identifying outpatients who meet criteria for CHR-P or psychotic disorder. Using this brief and simple psychosis screener in primary care, psychiatry outpatient settings, and referral pathways may facilitate early identification and intervention of a high-need clinical population.