Social Vulnerability & Access to Care for Psychosis: A Geospatial Analysis of Clinics in MA
Iqra Imam (1,2), James Green (2,3), Kelsey A. Johnson (1,2), Emily Gagen (3,4), Henry White (3), Jessica Stern (3), Margaret E. Guyer (5), Matcheri Keshavan (1,3,4)
1. Massachusetts Psychosis Network for Early Treatment (MAPNET), Boston, MA
2. Beth Israel Deaconess Medical Center, Boston, MA
3. Brookline Center for Community Mental Health, Brookline, MA
4. Harvard Medical School Department of Psychiatry, Boston, MA
5. Massachusetts Department of Mental Health, Boston, MA
Abstract
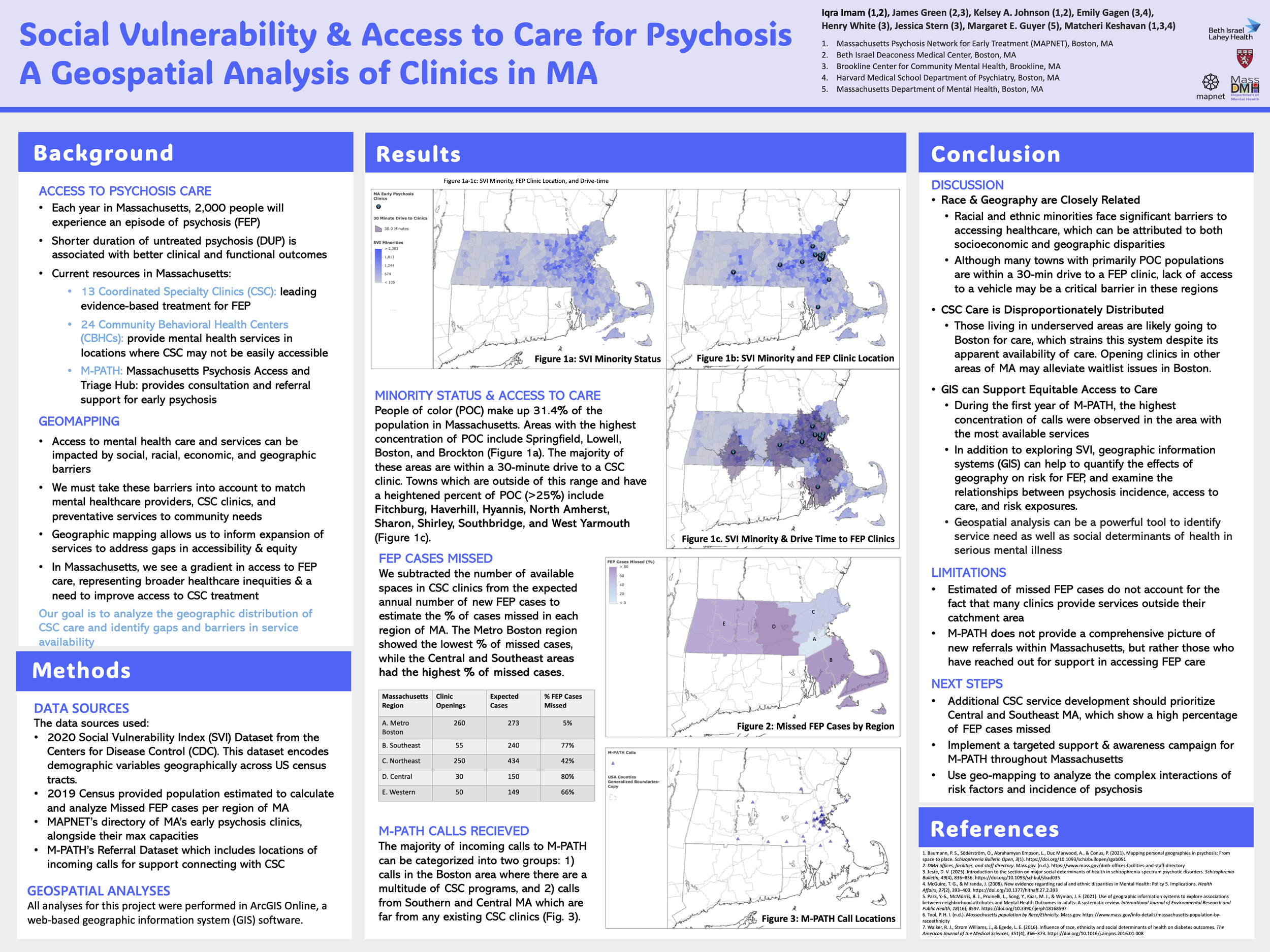
Background: Each year in Massachusetts, approximately 2,000 people will experience a first episode of psychosis (FEP). Shorter duration of untreated psychosis (DUP) is associated with better clinical and functional outcomes. In Massachusetts there are thirteen Coordinated Specialty Care (CSC) programs, which are the leading evidence-based treatment for FEP. In addition, there are 24 Community Behavioral Health Center (CBHC) locations, which serve in locations where CSC may not be easily accessible. Resources including the Massachusetts Psychosis Access and Triage Hub (M-PATH) provide consultation and referral support for early psychosis. This project aims to understand where care is being provided and examine gaps in service availability.
Methods: Maps were created in ArcGIS using the 2020 Social Vulnerability Index (SVI) dataset from the Centers for Disease Control (CDC), MAPNET 2023 FEP clinic directory, Massachusetts CBHC locations, M-PATH outreach data, and 2019 census data. These visualizations included the locations of the CSC clinics and CBHCs in located in Massachusetts, the maximum capacities of the CSC clinics, referrals received by M-PATH, and indicators of social vulnerability.
Results: The Boston area had both the highest number of FEP clinics and the highest maximum clinic capacities compared to other regions of Massachusetts. SVI shows higher concentrations in Worcester, Springfield, and Brockton. M-PATH calls were primarily received from individuals in the Boston Area, with most calls for the 15-25 age group. Highest FEP incidence is in Middlesex and Essex County.
Conclusions: Proper access to CSC is imperative. These analyses indicate that the current capacity of CSC clinics in MA is lower than what is needed to serve the expected incidence of FEP, identifying a need for policy improvement to meet the needs of this underserved population. Targeting geo-mapping data to focus on variables which may affect access to care, such as social determinants of health, may be a critical step to identify inequities and ensure equitable access to care.